A Comparative Study Analysis of Lower Limb and Upper Limb Conduction Velocity among Asymptomatic Patients of Type 2 Diabetes Mellitus
DOI:
https://doi.org/10.5530/jcram.1.1.6Keywords:
Diabetes Mellitus, Nerve Conduction Velocity, Nerve ConductionStudies, Peripheral Neuropathy, Diabetic Neuropathy, Sensory Nerve Conduction velocityAbstract
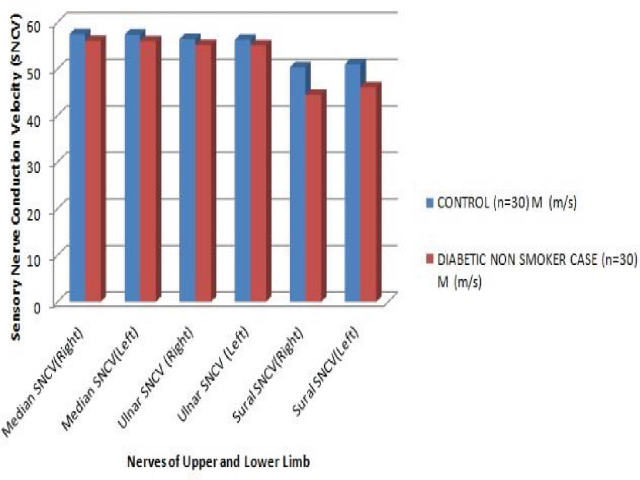
Objectives: Diabetes Mellitus is worldwide disease and diabetic peripheral neuropathy (DPN) is one of the most prevalent micro-vascular complication seen during the progress of disease. Frequently there is subclinical involvement seen for peripheral nerve functions which is revealed on nerve conduction study. Present study aims to assess nerve conduction velocity changes among asymptomatic patients with type 2 diabetes mellitus. Materials and Methods: Total 60 subjects were included for the study, 30 of them were of type 2 diabetes mellitus on regular treatment with disease duration of less than 5 years and asymptomatic for neuropathy and 30 were controls. All the participants were subjected to nerve conduction studies. Results: Nerve Conduction Velocity (NCV) of sural sensory nerve was found to be significantly decreased in diabetic patients as compared to controls. Conclusion: Sensory NCV was significantly decreased in the sural nerve compared to upper limb sensory nerves which suggests that long nerves are more prone to neuropathic changes even in asymptomatic diabetic patients.
Downloads
Published
How to Cite
Issue
Section
License
JCRAM and its contents are licensed under a Creative Commons Attribution-Non Commercial-No Derivs 4.0 License. Permissions beyond the scope of this license may be available with editor@jcramonline.com