Assessment of SOFA Score and its Relation with Sepsis Outcome in a Tertiary Care Centre
DOI:
https://doi.org/10.5530/jcram.1.2.13Keywords:
Sepsis, SOFA score, Systemic inflammatory response syndromeAbstract
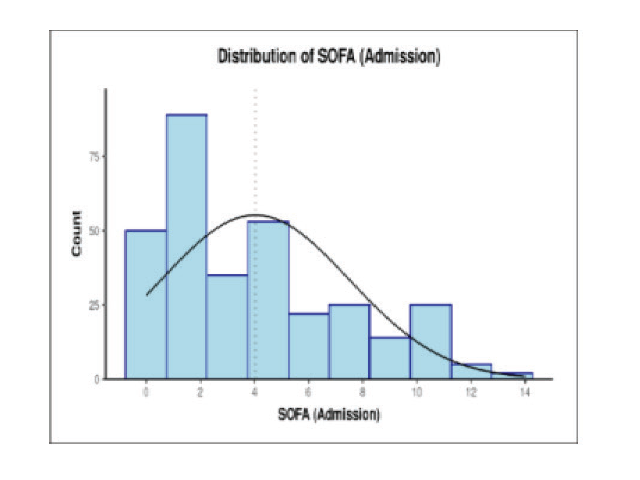
Aim: To study the association of SOFA score with sepsis and its correlation with patient outcome in a tertiary care centre. Materials and Methods: A prospective observational cohort study conducted on 320 patients of sepsis in Medicine department and ICU, SRN Hospital, MLN Medical College, Prayagraj, U.P. India. Results: In this study, out of 320 patients taken for the study 71 (22.2%) expired and 249 (77.8%) were discharged/referred. In the study, for mortality as an outcome (expired vs discharge), on the day of admission, day 3 and on day 7, the area under the ROC curve (AUROC) for SOFA at admission predicting Expired vs Discharged/Referred was 0.87 (95% CI: 0.819 - 0.921), thus demonstrating good diagnostic performance. It was statistically significant (p = <0.001). The relative risk (95% CI) for expired group, when SOFA on admission is ≥ 5 was 7.75 (4.8-12.63). PPV of 50.8% (42-60), NPV 95.0% (91-98) with diagnostic accuracy of 78.4% (74-83). Conclusion: In this study, it was seen that higher values of SOFA (at admission) scores was associated with poor outcomes. Higher rate of mortality was seen in all those subjects in whom persistent high values of SOFA scores were seen during the admission.
Downloads
Published
How to Cite
Issue
Section
License
JCRAM and its contents are licensed under a Creative Commons Attribution-Non Commercial-No Derivs 4.0 License. Permissions beyond the scope of this license may be available with editor@jcramonline.com